LYMPHEDEMA EDUCATION
Lymphedema can occur after many cancers including; breast cancer, melanoma, gynecologic cancer, head and neck cancer, sarcoma, and mesothelioma. Risk of lymphedema for all cancers is reported to be 15.5% while 32% of breast cancer patients report persistent swelling after surgery. The risk of developing lymphedema does not diminish over time but is a lifelong risk. Lymphedema is complicated by recurring infections, non-healing wounds, discomfort or pain, difficulty with activities of daily living, and emotional/ social distress. Effective treatment for lymphedema is available and early diagnosis is important since treatment is most effective when lymphedema is diagnosed at the earliest stage. Lymphedema has no cure but can be very successfully managed when properly treated by a licensed therapist. (Position Statement of the National Lymphedema Network TOPIC: The Diagnosis And Treatment Of Lymphedema 2011, Cancer Epidemiology, Biomarkers & Prevention 2007; 16(4): 775–82)
COMMON CAUSES of LYMPHEDEMA
★ Cancer Surgery
★ Lymph Node Removal
★ Radiation Treatment, .e.g., Breast Cancer, Head and Neck Cancers, Mesothelioma
★ Chronic Venous Insufficiency
★ Congenital Lymphedema ( Typically a malformation from birth)
★ Deep Vein Thrombosis (DVT)
★ A Tumor or Scar Tissue affecting/ compressing Lymphatics.
★ Filariasis
★ Sedentary Lifestyle/Morbid Obesity
★ Person confined to a wheelchair
★ Burns & Infections
WHAT IS LYMPHEDEMA?
Lymphedema is an accumulation of lymphatic fluid in the interstitial tissues. This causes swelling, most often in the arms and legs and to a lesser extent in the Head, Neck, and even Genitals. Lymphedema can present when the lymph vessels are dysfunctional. In Primary Lymphedema, the vessels are missing or developed improperly. In Secondary Lymphedema, the lymph vessels are damaged or removed-- often from surgery.
WHAT CAUSES LYMPHEDEMA?
Primary lymphedema can be present at birth or can develop spontaneously during different stages of life based on "triggers or stresses" to lymphatics. Wyatt has treated infants for this condition. Primary Lymphedema is also associated with vascular anomalies e.g., hemangioma, lymphangioma, Port Wine Stain, Klippel Trenaury.
Secondary lymphedema is acquired lymphedema where the lymphatics are typically impaired as a result of surgery, radiation, infection (e.g. lymphangitis) or trauma. This is especially true during lymph node removal or repeated aspirations of a seroma. Another cause of lower limb lymphedema is believed from the use of Tamoxifen. This medication can cause blood clots and subsequent deep venous thrombosis (DVT).
Aircraft flight has also been linked to lymphedema onset. Filariasis is a rare form of lymphedema seen in undeveloped countries from mosquito larvae. In Secondary Lymphedema, swelling can develop as early as immediately post-op or even years later.
LYMPHEDEMA SYMPTOMS
Some signs and symptoms to look for: a full sensation in the limb(s), skin feeling tight, decreased flexibility in the hand, wrist or ankle, difficulty fitting into clothing or jewelry.
Lymphedema Stages
(Note: The longer Lymphedema goes untreated, the harder it is to manage. It is considered a progressive condition. Later stages result in longer treatment to control swelling.)
Stage 1
Tissue is at the "pitting" stage, this means that when pressed by fingers, the area indents and holds the indent. In the morning the affected area appears near normal.
Stage 2
The affected area has a sponge texture and is "non-pitting", i.e., when pressed by fingers, the tissue rebounds without a persistent indent.
Stage 3
At this stage the there is tissue fibrosis, and skin changes/ infections. If left untreated severe consequences can occur, i.e., recurrent infections, soft tissue contractures, and progression.
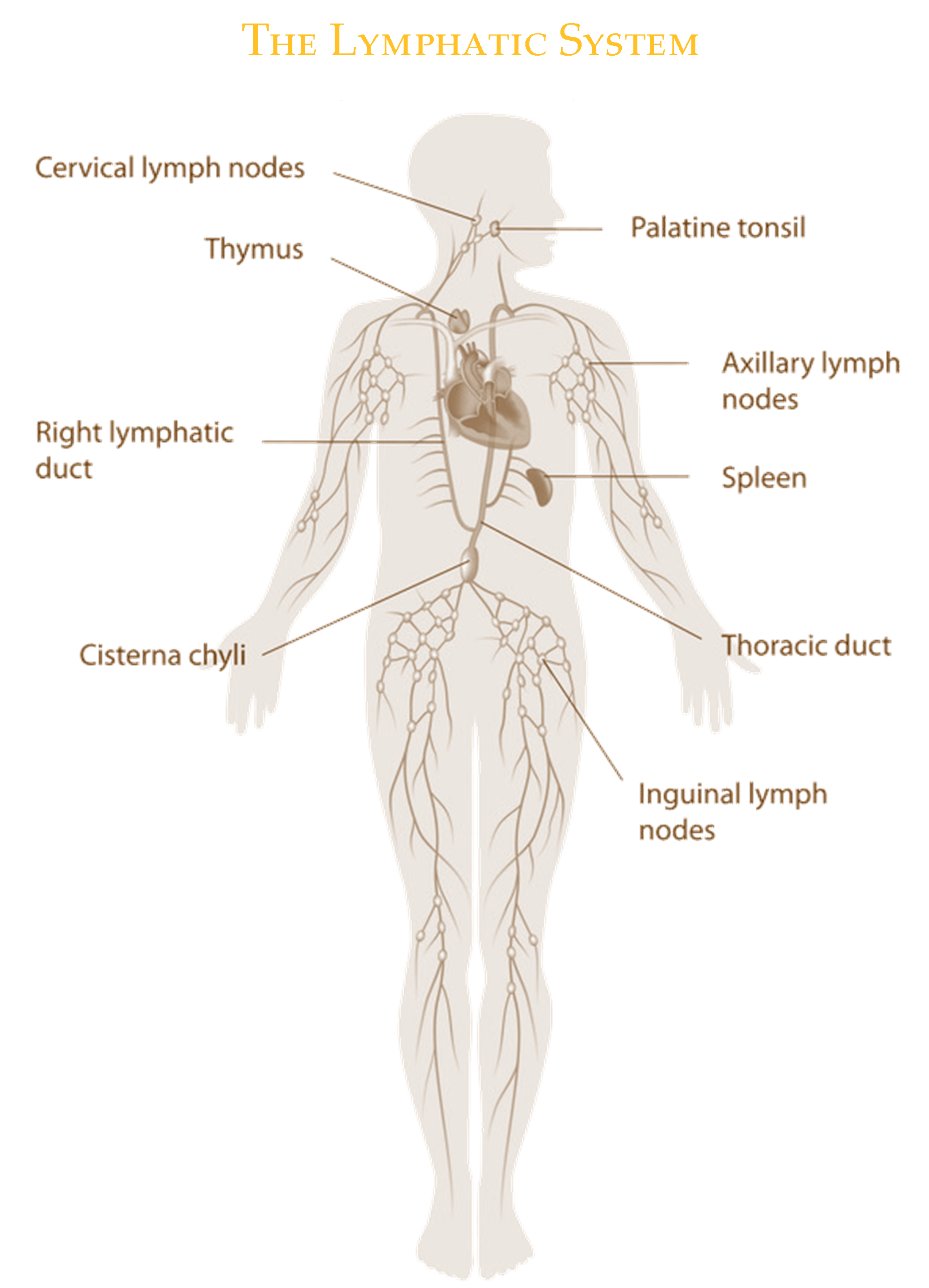
The Lymphatic System is composed of both circulatory and immune structures. Therefore Lymphedema is a condition of impaired lymphatic structures and immunity. The Lymphatic System is a low pressure system that regulates fluid homestasis and immune defense. Failure of any part of this system can affect fluid loads resulting in excess interstitium fluid "Lymph". We possess a main Circulatory System that moves blood from our heart out to our tissues. The Lymphatic System parallels this system capturing excess fluid and filtering it through our Lymph Nodes while conferring immune benefits. Lymphocytes are involved in immune defense and antibody production.
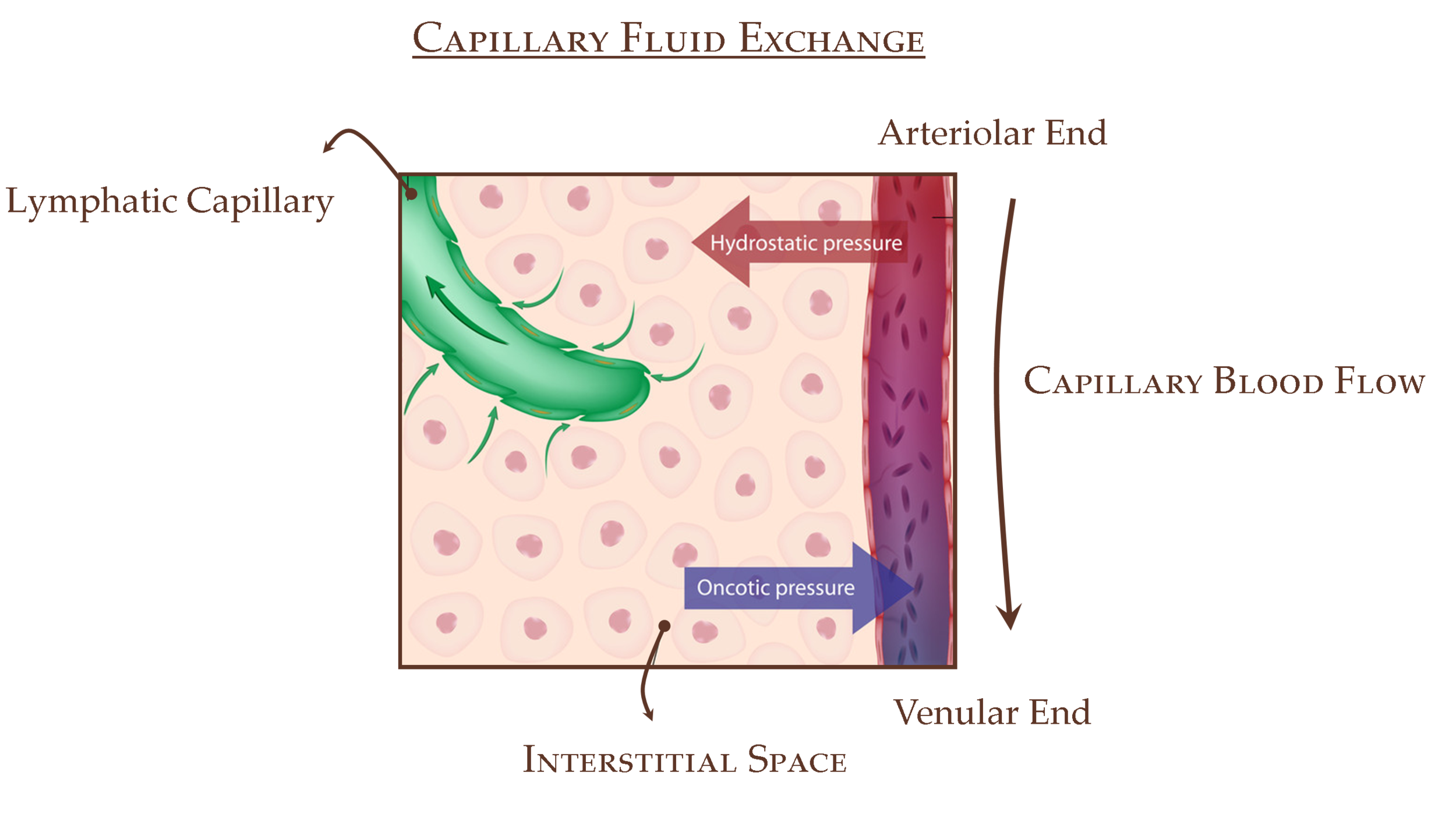
Capillary Pressure Drives Interstitial Fluid. This "vasomotion" pulses with our heart. This fluid is filled with water, lipids, antigens, immune cells, and particulate matter. The Interstitium is elastic and fibroblasts (via an integrin fiber network) actively control tissue pressure and therewith lymph formation. Fibroblasts are precursors to Collagen and Adipose (fat).
Blood Capillary walls are semipermeable and allow water and dissolved molecules to diffuse in both directions. Every minute, 240 ml diffuse through a meter of our capillaries. An ideal "laboratory" semipermeable membrane would not allow proteins to cross but capillaries do. This results in some proteins in the interstitial space. Protein molecules trickle through the interstitium toward the initial lymphatics. Movement of plasma proteins is a normal process and is constant. The osmotic pressure between interstitium and capillary is identical and in equilibrium in theory- "Starling Equilibrium" controlled by Osmotic, Interstitial, and Capillary pressures. Changes in this equilibrium lead to inflammation and lymphedema. In reality, this is a dynamic system- a Chemical and Mechanical Concert of filtration and resorption of fluid. Congenital malformations and surgical disruptions affect this system as do radiation and some parasites. In fact, post-operative Radiation increases risk of Lymphedema 10 fold versus surgery alone. (Foldi Textbook of Lymphedema 2003, Lee, Bergan and Rockson Lymphedema 2011)
MESOTHELIOMA is a cancer and as such may require radiation treatments and potential surgeries which could affect the lymphatic system. Manual Lymph Drainage can reduce lymphedema and swelling associated with these treatments. See this associated link regarding Lymph Drainage Therapy at Mesothelioma.com at our Link Page. "Some experts note that a course of manual lymph drainage (MLD) therapy shortly after surgery may assist in the development of collateral lymphatic circulation which can assist the patient in avoiding the condition altogether". (Mesothelioma.com)
American Journal of Medical Genetics Part A. Volume 152A ... 2010.Lipedema: An inherited condition
LIPEDEMA is a chronic fat metabolism disease that results in peculiar distribution and storage of fats due to genetic and hormonal abnormalities. It is predominately seen in women and has a familial component. It often does not affect the feet and is somewhat painful to touch. Fat distribution typically occurs symmetrically and almost exclusively from pelvis to ankle. In later stages of the condition, the skin can become "orange-peel" like and the excess fat can become large nodes with complications such as cellulitis. This condition typically progresses to Lymphedema or Lipolymphedema as the fat cells put pressure on lymph collectors and alter microcirculation creating conditions for swelling. "Active treatment for lipedema is required because early diagnosis and treatment can determine the patient's long-term prognosis." Complete Decongestive Therapy is used to reduce swelling and pain while Physical Therapy assists to improve function. 11% of women are reported to experience Lipedema.
(Annals of Rehabilitation Medicine 2011 December; 35(6): 922–927 www.e-arm.org)
LYMPHEDEMA TREATMENT
Our Lymphedema Treatment consists of consecutive therapy sessions to achieve an appropriate response in an involved area of swelling. Integral to the success of any lymphedema treatment program is an agreement between therapist and patient to work together toward the desired goal of improved limb function, appearance, and health. Lymphedema is a chronic condition which requires ongoing maintenance, care, and periodic expert supervision. Our patients receive individualized follow-ups throughout the year to ensure their results are maintained.
Credit: Lymphedivas
Complete Decongestive Therapy (CDT) is the most successful treatment for chronic lymphedema. Post- Mastectomy Lymphedema and other related conditions respond extremely well to this gentle, non-invasive, and highly effective therapy. CDT is sometimes referred to as Complete/Complex Decongestive Physiotherapy (CDP). CDT consists of the following steps:
1. Manual Lymph Drainage (MLD)
MLD is a very gentle manual treatment which improves the function of the lymphatic system throughout the body. In the 1930s the techniques of MLD were first introduced by Dr. Emil Vodder, PhD, MT, from Denmark. MLD is becoming widely recognized in the United States as a treatment for many pathologies including post surgical swelling, post traumatic edema (e.g., sports and other accidental injuries), and combined edemas such as phlebolymphostatic edema and lipo-lymphedema. MLD is further used to promote general relaxation, pain management, and the cleansing (detoxification) of the skin and superficial fascia. In lymphedema therapy, MLD is used to reroute the lymph flow around blocked areas into healthy lymph vessels which drain into the venous circulation.
2. Compression Therapy
Compression therapy, through the use of multilayered bandages, increases tissue pressure and is applied between treatments to prevent the re-accumulation of evacuated edema fluid. Compression therapy also increases the efficiency of the muscle and joint pumps and is used until the limb is sufficiently decongested to be fitted for compression garments.
3. Exercises
Remedial exercises, with the bandages in place, are performed to activate the muscle and joint pumps of the affected extremity. This results in an increase in lymphokinetic activity and, over time, in further reduction of the swollen limb.
4. Skin Care
Skin care and general hygiene are essential for eliminating bacterial and fungal growth, either of which can cause repeated attacks of cellulitis or erysipelas. Because infections are very common complications of lymphedema, meticulous skin and nail care are integral elements of CDT.
5. Patient Education
Because lymphedema management is an ongoing process, each patient is educated in a unique and specific program of self-care. Such a tailored treatment program ensures that each patient remains confidently in control of his or her lymphedema, decreasing reliance on continuous medical
LYMPHEDEMA PREVENTION:
In general, minimize air flight, minimize becoming overheated (think Spa/ Sauna), and excessive weight gain. When in doubt see Wyatt for a professional evaluation. While some variables you have no control over, there are certainly precautions to be taken. There have been many at risk patients, e.g., from breast cancer surgery and venous disorders, who developed lymphedema with flight and other risk factors. See our Testimonials for examples of highly Satisfied Patients.